Migraines are severe, throbbing headaches that may or may not be accompanied by nausea, visual disturbances, and other symptoms. The incidence of migraine headaches has increased by 50% within the last 20 years, with an estimated 5 million Australian’s suffering from them. 71% of migraine sufferers are women and 86% are of working age. Migraines are one of the most severe types of headache, with 8% of migraine sufferers experiencing chronic migraine more than 15 days per month.
Migraines go beyond the typical stress or allergy-related headache. Migraines last anywhere from 4 to 72 hours, and even the most mundane activities can amplify your symptoms. This includes being around noise and light; and moving. While pain killers can help alleviate migraine symptoms temporarily, there are concerns about their side effects. This is where CBD oil comes in. CBD is one of the many active compounds found in the cannabis plant. It is quickly growing in popularity as a way to treat migraines naturally.
One of the major benefits of CBD oil, especially for proponents of natural treatments, is the fact that CBD is not a pharmaceutically-engineered drug with a host of potential side effects and negative drug interactions. However, that is not where its benefits end.
CBD Oil is Legal!
It’s been widely touted in the news and is gaining wider acceptance as an effective treatment for migraine sufferers. We all want to know that what we’re putting in our bodies is safe. Drug companies have developed several effective migraine medications, however, for a large number of migraine sufferers drugs aren’t the ideal answer. Many of us would prefer something natural, but also effective. CBD oil has potential as a safe, natural treatment for migraine. Several studies have linked CBD oil with pain relieving properties, and also documented its safety.
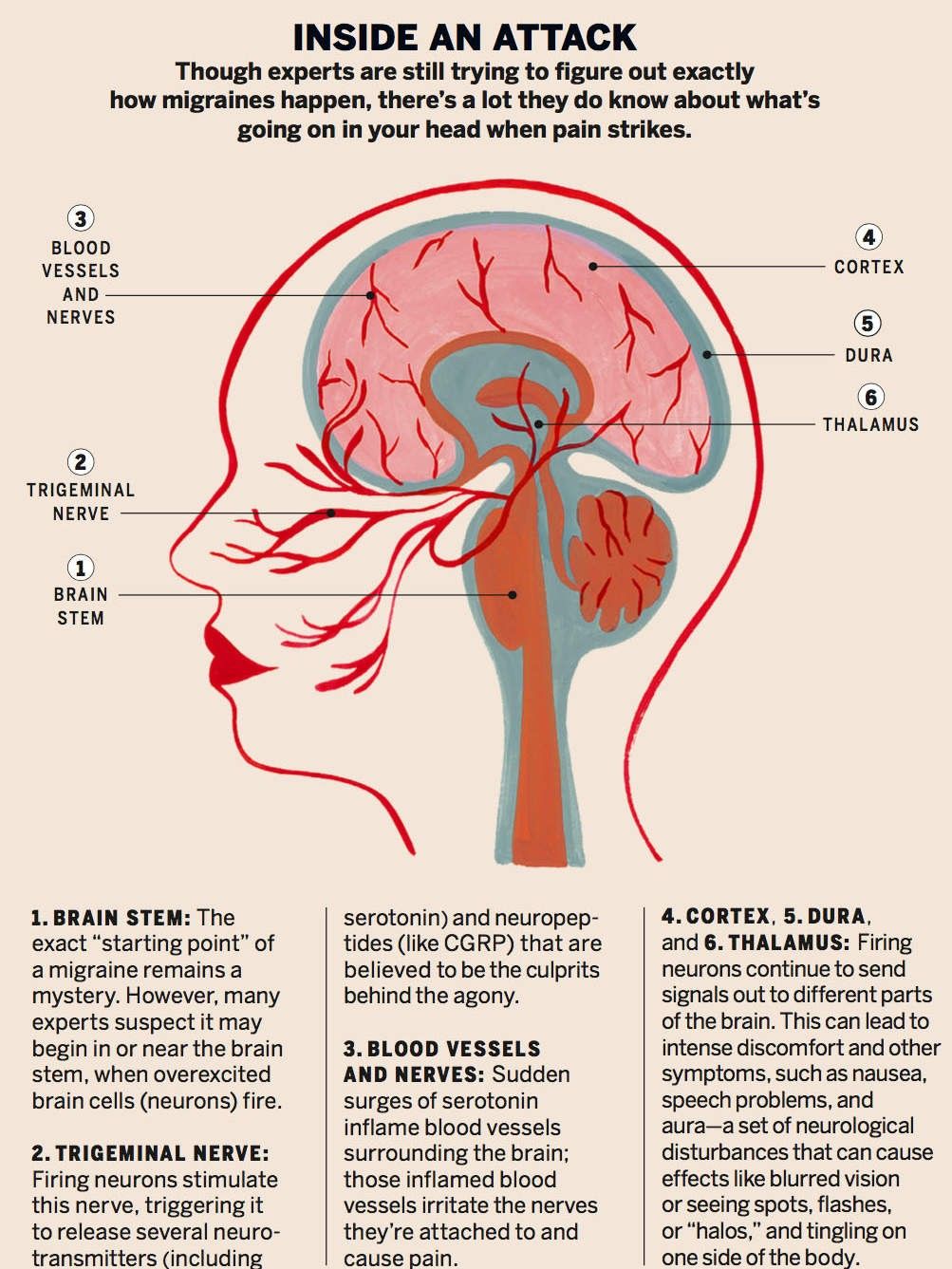
Traditional research has described migraines as vascular headaches involving excessive dilation or contraction of the brain’s blood vessels. More current research gives other clues. Single photon emission computerised tomography (SPECT) scanning indicates that the inflammation involved in migraines is not noticeable in the meninges. These are three membranes – the dura, the arachnoid, and the very inner layer of membrane, called the pia, which is separated from the other two by cerebrospinal fluid. These membranes surround the brain and the spinal cord.
However, it is not the inflammation of the meninges that leads to the pain of migraine, but rather abnormal nerve activity. Stimulation of the trigeminal nerve, which goes from the brain to the head and face, appears to trigger the release of substances known as calcitonin gene-related peptides (CGRP), which both induce inflammation and send message to pain receptors in the meninges. Some researchers liken migraines in many ways to meningitis, anther condition affecting the meninges, noting that with meningitis, the symptoms are very similar – headache, nausea, and sensitivity to light. Meningitis, however, is caused by a viral or bacterial infection.
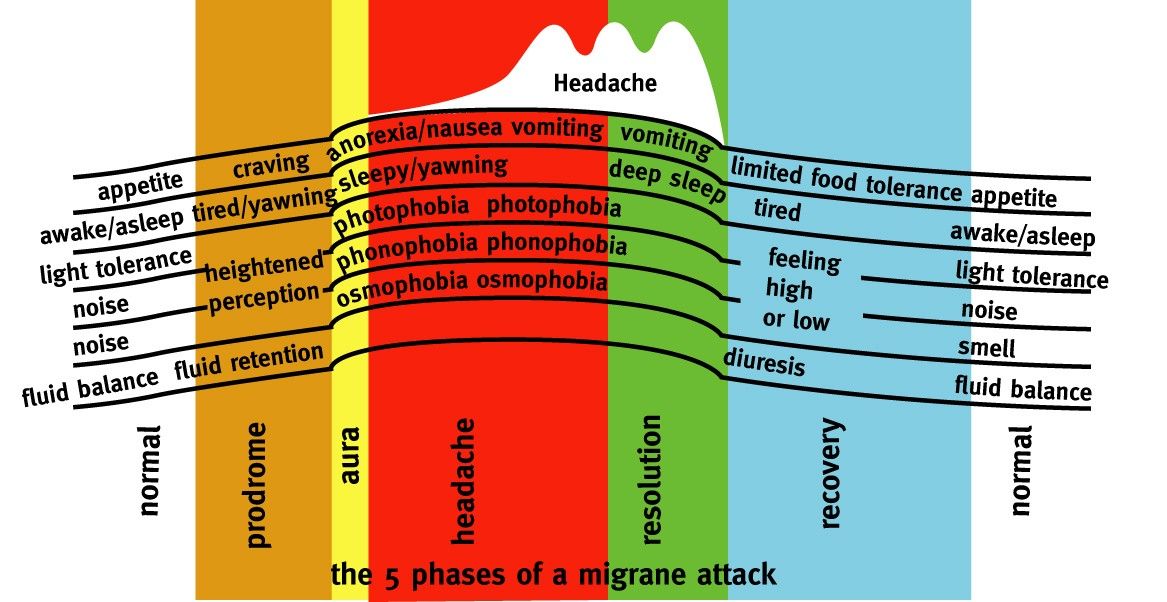
Migraines may occur anywhere from more than once a week to once or twice a year, and they often run in families. One factor behind the higher incidence of migraines in women may be fluctuations in the level of the hormone estrogen; women typically get migraines around the time of menstruation, when estrogen levels are low. Migraines occur most often in people between the ages of twenty and thirty-five, and tend to decline with age. However, children too can suffer from migraines. In children, migraine pain tends to be more diffuse, rather than localised. Migraines can first show up in childhood not as headaches, but as colic, periodic abdominal pains, vomiting, dizziness, and severe motion sickness. There are usually five phases in a migraine:
- A day or so before the onset of a headache, there may be detachable changes in mood, problems with memory, an alteration in one or all of the five senses, or speech problems.
- Just before the headache begins, some people see flashes or patterns of light and/or experience numbness of the hands or mouth. This is called an aura, much like the auras that affect many people with epilepsy before a seizure. A migraine preceded by an aura is called a classic migraine. Migraines without auras are called common migraines.
- The headache starts, with severe, throbbing pain. It may occur on one side or both sides of the head. The pain can also move from side to side. Nausea may set in, along with tenderness in the neck and scalp. The eyes may be very sensitive to light, and the person may be almost immobilised by the pain.
- The headache dissipates, nausea may linger, however.
- The person may feel tired and lethargic and may simply want to sleep.
Any number of things can trigger a migraine in a susceptible individual, including allergies, constipation, stress, liver malfunction, too much or too little sleep, emotional changes, hormonal changes, sun glare, flashing lights, lack of exercise, and changes in barometric pressure. Dental problems may also be a factor. Low blood sugar is frequently associated with migraine; studies have shown that blood sugar levels are low during a migraine attack, and the lower the blood sugar level, the more severe the headache. Underlying causes of migraines that render an individual susceptible to various immediate triggers can include genetic factors, chemical imbalances in the brain, poor nutrition, and the overuse of painkillers.
Considerations
Some researchers believe many migraine attacks are caused by chemical imbalances in the brain. Serotonin levels in the brain drop during a headache. This triggers an impulse along the trigeminal nerve to blood vessels in the meninges, the brain’s outer covering. In the meninges, the blood vessels become inflamed and swollen. The result is a headache.
In women, migraine frequency and severity are affected by hormones and, as a result, often change during adolescence, pregnancy and menopause. Beginning around menarche (the first menstrual cycle), its prevalence increases during reproductive years and then decreases around menopause. Women often experience an improvement in migraine during pregnancy, however, unfortunately it typically reappears following birth. After about 70 years of age the prevalence of migraine decreases to that of the middle teen years.
Source: Headache Australia www.headacheaustgralia.org.au
There are a number of common misdiagnoses of headache, including sinus pain, allergies and temporomandibular joint syndrome (TMJ). What many people think are sinus headaches are really migraines. Sinus infections can cause brief, intense bouts of head pain, but recurring headaches are more likely to be tension headaches, migraines, or cluster headaches. Facial pain, pain in the temples, or pain above the ear is sometimes diagnosed as TMJ headache, caused by the joint of the jawbone being out of alignment. Poor vertebral alignment may cause reduced blood flow to the brain, this is often caused by flat feet, or by wearing high heels.
Call a doctor if you have a headache that is triggered by, accompanied by, or linked to, any of the following:
- Exertion (including sexual exertion), bending, or coughing
- Stiff neck and fever
- Head injury
- Vomiting
- Slurred speech, distorted vision, or numbness or tingling in part of the body
These can be triggers of more serious disorders
Distinguishing Migraine Headaches
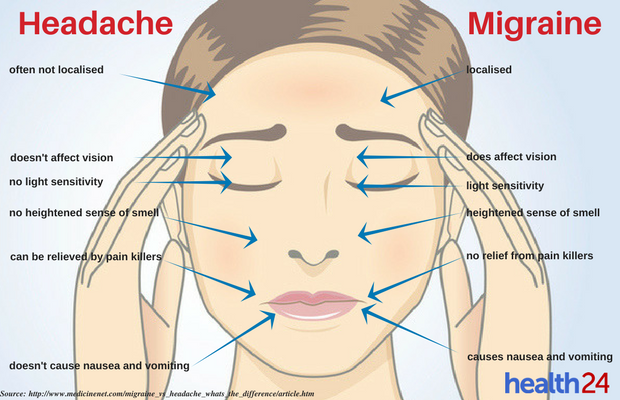
Just because a headache is very painful, does not mean it is a migraine. Migraines have certain characteristics that set them apart from other types of headaches. Two types of headache most commonly confused with migraines are tension or cluster headaches.
Tension Headaches
Tension Headaches are dull, tightness, or pressure around your forehead or the back of your head and neck. Often described as feeling like a clamp squeezing the skull. Sometimes called Stress Headaches, they’re the most common type for adults. Tension headaches are caused by muscle contractions in the head and neck regions. A variety of foods, activities, and stressors can cause these types of contractions. Some people develop tension headaches after staring at a computer screen for a long time, or after driving for long periods.
There are two types:
- Episodic Tension Headaches occurring less than 15 days per month. These can last from 30 minutes to a few days. The episodic type usually start gradually, often in the middle of the day.
- Chronic Tension Headaches occurring more than 15 days per month. Chronic headaches come and go over a longer period of time. The pain may get stronger or ease up throughout the day, but it is almost always there.
Cluster Headaches
Cluster headaches are a series of relatively short but extremely painful headaches every day for weeks or months at a time. They tend to occur at the same time each year, such as spring or autumn. Because of their seasonal nature they are often mistaken for symptoms of allergies or executive stress. The exact cause of cluster headaches is unknown, but cluster headache patterns suggest that abnormalities in the body’s biological clock play a role. Unlike migraine and tension headaches, cluster headaches generally aren’t associated with triggers such as foods, hormonal changes or stress. We don’t know what causes them, but we do know that a nerve in your face in involved, creating intense pain around one of your eyes. It is so painful that most people can’t sit still and will often pace during an attack. Cluster headaches can be more severe than a migraine, but they usually don’t last as long.
Cluster headaches are the least common type of headaches, affecting less than 1 in 1,000 people. Men get them more than women, usually beginning before the age of 30. Cluster headaches may disappear completely, or go into remission for months or years, but they can return without any warning.
An article published in 2018 in Frontiers of Neurology discussed evidence that CBD has a number of positive pharmacological properties, including as an anti-inflammatory, anti-oxidative, antiemetic, antipsychotic, and neuro-protective substance. CBD has been explored in the treatment of migraines, and the study cites the fact that CBD is safe, as it does not alter heart rate, blood pressure and body temperature, and psychomotor and psychological functions are not negatively affected. With its safety established, many migraineurs feel secure about trying CBD oil to treat their migraines.
Medications and natural methods of pain relief work differently for different individuals and CBD oil is no exception. By testing out pure CBD oil and assessing its effects on you personally, you can determine if it is an effective natural pain reliever for you and your symptoms. As migraine sufferers continue to search for relief that won’t overload their bodies with pharmaceuticals, science continues to rise to the challenge. With a track record of safety and non-addictive nature, CBD oil is definitely worth a try for many migraine sufferers.
Can CBD Oil help me with my Migraines?
Many people ask the same questions. And the short answer is YES! There have been many studies showing promising results when evaluating cannabis for its effects on chronic pain and inflammation, however, we are still waiting on documented studies of CBD and its specific effect on migraines. Many sufferers are trying it for themselves and a “study of one – ie: You”; is the best way to find out how CBD oil can benefit you. Feedback to date tells us that CBD oil helps to ease migraine pain, and even shorten attacks. Using CBD to treat headaches is not new. As an ancient natural remedy, cannabis has been used for thousands of years to treat certain types of headaches. The type of cannabis that CBD is composed of is very well tolerated and safe in humans, with no nasty side effects (including psychotic symptoms).

Queen Victoria’s personal physician is believed to have used cannabis to ease the monarch’s severe menstrual cramps and migraines.
Cannabis continued to be prescribed in western medicine until 1937 when the United States introduced the Marijuana Tax Act. While not yet criminalising its use, this Act placed such a high tax on cannabis products (allegedly due to lobbying by the petrochemical industries who viewed pharmaceutical cannabis as a competitor) that production largely ceased.
By 1961, the United Nations Single Convention of Narcotic Drugs, placed marijuana in its most restrictive category, Schedule IV, effectively labelling cannabis a poison.
Properties of CBD Oil which relieve Migraine
- Potent analgesic (pain relieving) properties
- Antiemetic (preventing nausea and vomiting) properties
- Powerful anti-inflammatory effects
How is CBD oil administered?
- As an ingredient in food or drinks
- In capsule form
- By inhaling or vaping
- As a topical application for the skin
- In drops or sprays used in the mouth
Because there are so few studies involving humans in the investigation of the effects of CBD oil on migraines, there is no standard dosage or method. The best recommendation is to start on a very low dosage and see if it is effective.
At iCannabis we are focused on bringing the purest and most bioavailable medical cannabis to Australian patients and their families.We are a group that specialises in educating and helping Australia patients gain access to Cannabis for Medical purposes. Through education and real-life experiences with the healing powers of this plant.
Once you discover the documented benefits tens of thousands of patients around the world have received from the medicine, you too will realise how this can potentially change and improve the lives of you and your family.The positive impact this plant has already had on the quality of life for patients and their families is nothing short of miraculous. At iCannabis we are committed to establishing an Australian medical cannabis community comprised of passionate and caring people, focused on the highest quality organic medicine made with love and integrity.
If you need any advice or help with CBD Migraine care or sourcing full spectrum cannabis oil treatments please contact us. We try to answer all emails within 24 hours and are happy to help and advise on all aspects of CBD treatments in complete confidence.
